
I’ve always been fascinated by numbers, especially those related to health. Recently, I stumbled upon a startling statistic: according to the World Health Organization, 39% of adults worldwide were overweight in 2016. This got me thinking about Body Mass Index (BMI) and its significance in our lives. As someone who’s struggled with weight fluctuations, I decided to dive deep into the world of BMI. Here’s what I discovered.
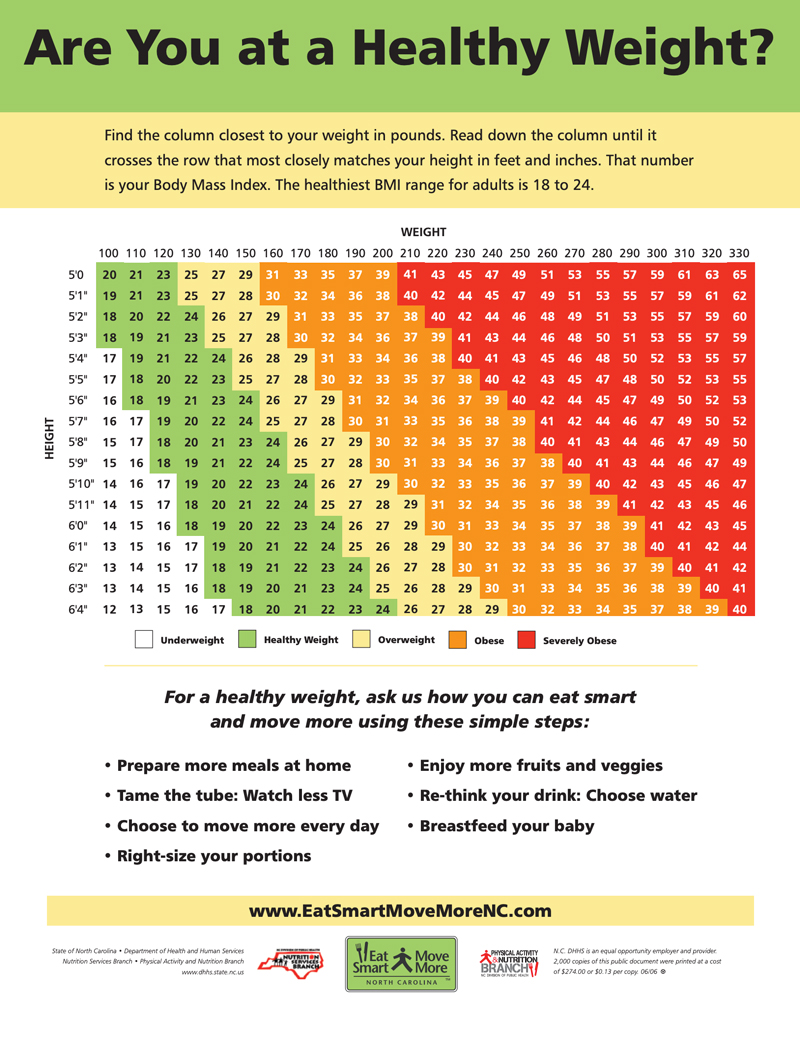
BMI is a simple yet powerful tool used to assess body composition. It’s calculated by dividing weight in kilograms by height in meters squared (kg/m²). The World Health Organization classifies BMI ranges into distinct categories: underweight (<18.5), normal weight (18.5-24.9), overweight (25-29.9), and obese (≥30). These classifications help healthcare professionals and individuals gauge potential health risks associated with body weight.
However, it’s crucial to understand that BMI isn’t a perfect measure. One significant limitation is its inability to distinguish between muscle mass and fat. This can lead to misclassification in certain populations, particularly athletes or individuals with high muscle mass. Despite this drawback, BMI remains a widely used metric due to its simplicity and accessibility.
In the United Kingdom, the impact of BMI on public health is substantial. According to the NHS, it’s estimated that around 1 in every 4 adults and around 1 in every 5 children aged 10 to 11 are living with obesity. These statistics highlight the importance of understanding and monitoring BMI as part of overall health management.
The Evolution of BMI
The journey of BMI spans centuries, from a Belgian mathematician’s curiosity to a global health standard. It’s a fascinating evolution that has shaped how we understand and measure body composition today.
Adolphe Quetelet, a Belgian polymath, developed the precursor to BMI in the 19th century. His work laid the foundation for what we now know as Body Mass Index. Quetelet wasn’t just interested in body measurements; he was a renaissance man whose work spanned astronomy, statistics, and social sciences. His multidisciplinary approach led to the creation of the Quetelet Index, which would later evolve into BMI.
Quetelet’s original formula, known as the Quetelet Index, was weight divided by height squared. He believed that the relationship between height and weight could be mathematically expressed. Interestingly, Quetelet’s formula was initially used to study population-level trends, not individual health.
The term “Body Mass Index” itself wasn’t coined until much later. In 1972, Ancel Keys introduced the term, marking a significant milestone in the metric’s history. From there, BMI began its journey towards becoming a global standard for assessing body composition.
The World Health Organization played a crucial role in transforming BMI from a statistical tool to a global health standard. In the 1980s, the WHO adopted the modern BMI formula, establishing international cut-off points in 1995. These standards were further refined in 2000 to include more specific categories for Asian populations, acknowledging the need for population-specific considerations.
Source: Wikimedia Commons
Consider a person weighing 70 kg and standing 1.75 m tall. Using Quetelet’s original formula, their BMI would be calculated as 70 / (1.75 * 1.75) = 22.86, placing them in the normal weight category. This simple calculation demonstrates the enduring relevance of Quetelet’s work, even as our understanding of body composition has evolved.
The digital age has revolutionized how we calculate and interpret BMI. Online BMI calculators have made it easy for individuals to assess their BMI instantly. Mobile apps now integrate BMI tracking with other health metrics for a more comprehensive view of personal health. Even more impressively, machine learning algorithms are being used to improve BMI interpretation based on individual factors.
Artificial Intelligence is taking BMI analysis to new heights. AI models can now factor in age, gender, and ethnicity for more accurate BMI interpretation. Some AI systems can even suggest personalized interventions based on an individual’s BMI and other health data. This level of personalization marks a significant advancement from Quetelet’s original population-level approach.
Wearable technology has made it possible to track BMI in real-time. Smartwatches and fitness trackers now offer continuous monitoring, providing insights into how our BMI fluctuates throughout the day and over time. Some wearables use bioelectrical impedance analysis to estimate body fat percentage alongside BMI, offering a more nuanced view of body composition.
Source: Google Play Store
Curious about how your BMI stacks up? Check out our guide on how to calculate BMI accurately for a step-by-step breakdown.
Beyond the Number: BMI’s Multidimensional Impact
BMI isn’t just a number on a chart. It’s a metric that influences various aspects of our lives, from our self-perception to public health policies. The implications of BMI extend far beyond personal health, shaping societal structures and individual experiences in profound ways.
In epidemiological studies, BMI serves as a crucial tool for assessing population health trends. Researchers use BMI data to track obesity rates, identify at-risk populations, and evaluate the effectiveness of public health interventions. This population-level application of BMI helps inform policy decisions and resource allocation in healthcare systems worldwide.
Insurance companies often use BMI as a factor in determining premiums. This practice has sparked debates about fairness and discrimination, highlighting the complex interplay between health metrics and economic factors. While BMI can provide valuable health risk information, its use in insurance calculations raises questions about the broader societal implications of body composition measurements.
The relationship between BMI and socioeconomic factors is complex and often surprising. In developed countries, studies show a correlation between lower socioeconomic status and higher BMI. This trend points to broader issues of food access, education, and healthcare disparities. Conversely, in some developing nations, higher BMI is associated with higher socioeconomic status, challenging our assumptions about wealth and health.
This BMI paradox in developing nations is particularly intriguing. As economies grow, so do BMI levels in many cases. Rapid urbanization often leads to increased access to processed foods, while economic growth can lead to more sedentary lifestyles. Cultural factors, such as perceptions of body size as a sign of prosperity, can also influence BMI trends in these contexts.
BMI’s impact extends into the psychological realm as well. Studies show a correlation between BMI and mental health issues such as depression and anxiety. The way BMI is communicated by healthcare providers can significantly impact patient well-being, underscoring the need for sensitive and nuanced approaches to body composition discussions.
| BMI Category | Health Risks | Recommended Actions |
|---|---|---|
| Underweight (<18.5) | Nutritional deficiencies, osteoporosis | Consult with a nutritionist, increase calorie intake |
| Normal weight (18.5-24.9) | Lowest risk for health issues | Maintain healthy lifestyle |
| Overweight (25-29.9) | Increased risk of cardiovascular disease | Moderate weight loss, increase physical activity |
| Obese (≥30) | High risk of type 2 diabetes, heart disease | Significant weight loss, medical supervision |
The psychological impact of BMI extends to body image and self-esteem. BMI categorization can significantly influence how individuals perceive themselves and their bodies. This influence is particularly pronounced in cultures where specific body types are idealized. The media’s representation of “ideal” BMIs can have a profound impact on body image, especially among young people.
Cognitive biases play a role in how we interpret BMI information. People often underestimate their own BMI, a phenomenon known as “BMI misperception.” This bias can lead to a disconnect between actual health risks and perceived health status. Cultural norms further complicate this picture, influencing how individuals perceive different BMI categories across various societies.
In the realm of policy and legislation, BMI’s influence is substantial. Many countries use population BMI data to inform national health policies, shaping everything from school lunch programs to public health campaigns. Some employers have incorporated BMI into wellness programs, raising ethical and legal questions about privacy and discrimination.
BMI has even found its way into legal cases related to discrimination and disability claims. These cases highlight the complex intersections between health metrics, individual rights, and societal norms. As our understanding of body composition evolves, so too must our legal and ethical frameworks for addressing BMI-related issues.
Recent developments in BMI trends offer a glimmer of hope. According to Science Alert, “US Obesity Rates Decline for the First Time in More Than a Decade”. Both average BMI and obesity rates across the US population fell in 2023, having risen steadily since 2013 before leveling in 2022. This shift suggests that public health initiatives and increased awareness may be starting to have a positive impact.
Looking to improve your BMI through dietary changes? Our comprehensive guide to meal planning can help you create a balanced eating strategy tailored to your goals.
The Biomechanics of BMI
BMI isn’t just about numbers on a scale. It has real, physical impacts on how our bodies function. The biomechanical aspects of BMI offer fascinating insights into its effects on our physical well-being, from joint stress to cardiovascular dynamics.
One of the most significant biomechanical impacts of BMI is on our joints. Higher BMI is associated with increased mechanical stress on weight-bearing joints, particularly the knees and hips. For every pound of body weight, 3-6 pounds of pressure is added to the knee joints during walking. This additional stress can lead to accelerated wear and tear on joint cartilage, potentially increasing the risk of osteoarthritis.
BMI can also affect posture and movement patterns, potentially leading to musculoskeletal issues. Individuals with higher BMI often adopt compensatory movement strategies to manage the additional body weight, which can result in altered biomechanics and increased risk of injury.
Source: ResearchGate
The impact of BMI on gait is particularly interesting. Higher BMI is associated with slower walking speed and shorter stride length. A gait analysis study found that individuals with a BMI over 30 had an average walking speed 0.16 m/s slower than those with a BMI under 25, demonstrating the tangible impact of BMI on mobility.
Individuals with higher BMI often have a wider base of support when walking, a strategy that enhances stability but may also increase energy expenditure. This increased energy cost during movement can affect overall physical activity levels, potentially creating a cycle where higher BMI leads to reduced activity, which in turn can contribute to further weight gain.
The spine also bears the brunt of increased BMI. Higher BMI increases the load on intervertebral discs, potentially leading to disc degeneration over time. Excess abdominal fat can alter the spine’s natural curvature, affecting posture and spinal health. On the positive side, weight loss can reduce spinal load, potentially alleviating back pain in individuals with high BMI.
BMI’s impact extends beyond our musculoskeletal system to our cardiovascular dynamics. Higher BMI is associated with increased blood volume and cardiac output. The heart must work harder to pump blood through a larger body mass, which can lead to left ventricular hypertrophy, a thickening of the heart’s main pumping chamber.
Source: YouTube
BMI also affects blood viscosity, or the thickness of blood. Higher BMI is associated with increased blood viscosity, which can affect blood flow and oxygen delivery to tissues and organs. This change in blood properties may contribute to the increased cardiovascular risk associated with higher BMI.
Understanding these biomechanical impacts of BMI can be crucial for developing effective interventions. For instance, weight loss programs that focus on gradual, sustainable changes can help reduce joint stress and improve cardiovascular health without putting undue strain on the body.
It’s important to note that while BMI provides valuable insights into potential biomechanical challenges, it doesn’t tell the whole story. Factors like muscle mass, fat distribution, and overall fitness level also play significant roles in how BMI impacts an individual’s physical functioning.
Redefining BMI: Alternative Approaches
As our understanding of body composition evolves, so must our metrics. While BMI has been a staple in health assessment for decades, its limitations have spurred the development of alternative measures. These innovative approaches aim to provide a more nuanced view of body composition and health risk.
The Body Adiposity Index (BAI) presents a fresh perspective on body composition assessment. Unlike BMI, BAI utilizes hip circumference and height to estimate body fat percentage. This method doesn’t require weight measurement, which can be advantageous in certain settings where scales may not be available or appropriate.
BAI’s use of hip measurements is particularly intriguing. Hip circumference is considered a more reliable indicator of body fat than weight alone, and the ratio of hip circumference to height offers insights into fat distribution that BMI might overlook. This can be especially valuable in assessing health risks, as fat distribution patterns can be as important as overall fat percentage.
Another alternative is BMI Prime, which introduces a novel approach to interpreting BMI values. BMI Prime is calculated by dividing BMI by 25 (the upper limit of the “normal” BMI range). This results in a more intuitive scale, with a BMI Prime of 1.0 corresponding to a BMI of 25. Values below 1.0 are classified as “underweight” or “normal weight,” while values above indicate overweight or obesity.
BMI Prime values typically range from about 0.60 (severely underweight) to 2.00 or more (morbidly obese). This scale can be particularly useful for setting weight loss goals and monitoring progress. For example, a BMI Prime of 1.2 would indicate that an individual is 20% over their ideal weight, providing a clear target for health improvements.
The Waist-to-Height Ratio (WHtR) offers yet another lens through which to view body composition. Determined by dividing waist circumference by height, WHtR focuses on central obesity, which is strongly linked to metabolic syndrome and cardiovascular risk. A WHtR of 0.5 or less is generally considered healthy for most adults.
WHtR is particularly effective for
WHtR is particularly effective for evaluating visceral fat, the metabolically active fat stored around organs in the abdominal cavity. Research suggests WHtR may be more sensitive than BMI in detecting cardiovascular risk factors, making it a valuable tool in health assessment.
| Metric | Formula | Advantages | Limitations |
|---|---|---|---|
| BMI | Weight (kg) / Height (m)² | Simple, widely used | Doesn’t distinguish fat from muscle |
| Body Adiposity Index (BAI) | Hip circumference / Height^1.5 – 18 | Doesn’t require weight measurement | Less studied than BMI |
| Waist-to-Height Ratio | Waist circumference / Height | Good indicator of central obesity | May not account for overall body composition |
| Body Fat Percentage | Various methods (e.g., DEXA, calipers) | Directly measures fat content | Can be costly or invasive |
Each of these alternative metrics offers unique insights into body composition and health risks. While they address some of BMI’s shortcomings, it’s important to note that no single measure provides a complete picture of health. A comprehensive approach often involves combining multiple metrics with other health indicators.
Source: ResearchGate
Recent developments in body composition assessment have seen the integration of advanced technologies. Bioelectrical impedance analysis (BIA) devices, for instance, send a small electrical current through the body to estimate fat and muscle mass. While these methods offer more detailed insights, they often require specialized equipment and trained personnel.
The future of body composition assessment likely lies in personalized, multi-faceted approaches. Artificial intelligence and machine learning algorithms are being developed to analyze various body measurements, lifestyle factors, and genetic data to provide highly individualized health assessments.
Despite the emergence of these alternatives, BMI remains a widely used metric due to its simplicity and accessibility. However, healthcare professionals increasingly recognize the need to consider BMI alongside other measures for a more comprehensive health evaluation.
Source: Dreamstime
Interestingly, recent data suggests positive trends in BMI and obesity rates. News Medical reports that “Obesity prevalence and BMI decrease in the US for the first time in a decade”. This decline, particularly notable in southern states, offers hope that public health initiatives and increased awareness are making an impact.
As we navigate the complexities of body composition assessment, it’s crucial to remember that these metrics are tools, not definitive judgments of health or worth. They provide valuable insights, but should always be considered in the context of overall health, lifestyle, and individual circumstances.
For those looking to optimize their body composition, personalized approaches often yield the best results. MealstoGlow’s AI-powered meal planner offers customized nutrition solutions that consider your unique body composition and health objectives. Whether you’re aiming to improve your BMI, enhance your WHtR, or simply adopt healthier eating habits, tailored nutrition plans can support your journey to better health.
Interested in exploring alternatives to BMI? Our article on advanced weight loss calculations delves into more sophisticated methods for assessing body composition and health.
In conclusion, while BMI has been a cornerstone of health assessment for decades, the field of body composition analysis continues to evolve. By understanding the strengths and limitations of various metrics, we can make more informed decisions about our health and well-being. Remember, the goal isn’t to achieve a perfect number, but to cultivate overall health and vitality.
Key Insights
- BMI serves as a widely utilized but imperfect measure of body composition
- Alternative metrics like BAI, BMI Prime, and WHtR provide more nuanced approaches to assessing body composition
- Understanding the biomechanical and cardiovascular impacts of BMI can inspire healthier lifestyle choices
- The psychological and societal implications of BMI underscore the need for a holistic approach to health
- Personalized nutrition, such as that offered by MealstoGlow, can support individuals in achieving and maintaining a healthy body composition
Ready to transform your health beyond just BMI? Explore our personalized meal plans designed to support your unique nutritional needs and health goals.





Add comment