
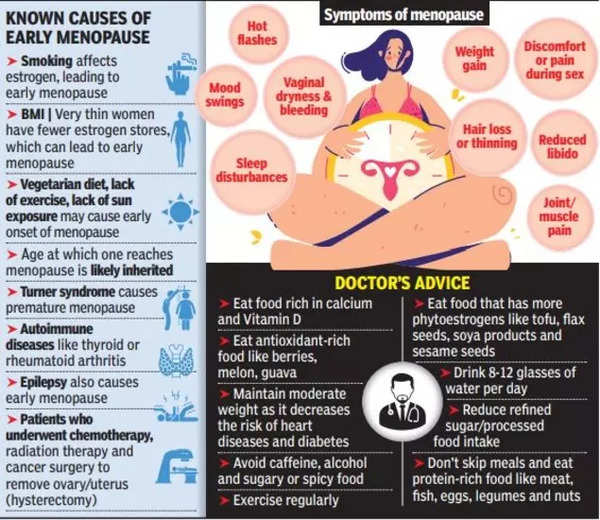
I remember the day I first noticed changes in my body that didn’t quite align with my age. At 45, I was caught off guard by symptoms I couldn’t immediately explain. Recent studies show that approximately 5% of women experience early menopause between ages 40 and 45. This unexpected life transition can affect multiple body systems, including reproductive, skeletal, and cardiovascular health.
Early menopause, defined as the onset of menopause between ages 40-45, presents a unique set of challenges compared to the average menopausal age of 51. The hormonal changes during this time can have far-reaching effects, impacting not just reproductive health but also bone density, heart health, and cognitive function. Early diagnosis and management are crucial for long-term health outcomes.
The rate of hormonal changes in early menopause can be more rapid than in natural menopause, potentially intensifying symptoms. Estrogen receptors are present in multiple tissues throughout the body, including the brain, bones, and cardiovascular system. As estrogen levels decline, these various systems can be affected in ways that might not be immediately obvious.
According to the NHS, approximately 5% of women naturally go through early menopause before the age of 45 [NHS Inform]. This statistic underscores the importance of awareness and early detection. Yale Medicine experts have recently discussed the health effects of menopause before age 45, highlighting the need for specialized care and attention for women experiencing this transition [Yale Medicine].
Source: Times of India
For those navigating early menopause, nutrition plays a crucial role in managing symptoms and supporting overall health. Exploring a low sugar meal plan can help manage some symptoms of early menopause, such as mood swings and fatigue.
The Biological Clock’s Curveball
Early menopause at 45 isn’t just an inconvenience; it’s a significant shift in your body’s timeline. This change brings a unique set of challenges and considerations that differ from those experienced by women who reach menopause at the average age of 51. Understanding these differences is crucial for managing your health and well-being effectively.
The onset of early menopause can accelerate age-related health risks typically associated with postmenopausal women. This means that conditions we often associate with older age might appear earlier than expected. It’s not just about hot flashes and mood swings; early menopause can affect your bone health, heart health, and even cognitive function in ways you might not anticipate.
Another significant aspect of early menopause is its impact on fertility. The shortened reproductive window may necessitate earlier discussions about family planning. For women who haven’t completed their families or were considering having children later in life, this can be a particularly challenging aspect of early menopause.
Sarah, a 43-year-old marketing executive, noticed her periods becoming irregular and experienced unexpected hot flashes during important meetings. Initially attributing it to stress, she soon realized these were early signs of menopause, prompting her to seek medical advice and adjust her health management strategies.
The Estrogen Enigma
Estrogen plays a pivotal role in early menopause, affecting numerous bodily systems. Its decline can trigger a cascade of changes, some obvious and others more subtle. Recognizing these changes is key to addressing them effectively and maintaining your overall health.
The rate of estrogen decline in early menopause can be more rapid than in natural menopause, potentially intensifying symptoms. This accelerated decline can lead to more pronounced effects on various body systems. Estrogen’s role in neuroprotection and cognitive function becomes compromised earlier in women experiencing early menopause, which can have implications for brain health and cognitive performance.
Research indicates that women experiencing early menopause may lose up to 20% of their bone density in the first 5-7 years after onset [Yale Medicine]. This rapid bone loss highlights the importance of early intervention and bone health strategies for women going through early menopause.
Source: Stanford Medicine
Cognitive Conundrums
You might notice changes in your cognitive function that seem out of place for your age. These can include difficulties with memory and concentration. While often attributed to stress or aging, these symptoms may actually be early signs of menopause-related estrogen decline.
Estrogen modulates neurotransmitters like serotonin and acetylcholine, which are crucial for cognitive function. As estrogen levels decrease, you might find yourself struggling with tasks that used to come easily. This isn’t just “normal aging” – it’s a direct result of hormonal changes.
Hippocampal function, essential for memory formation, can be affected by declining estrogen levels. You might notice that you’re more forgetful or have trouble recalling recent events. This isn’t a sign of early dementia; it’s often a symptom of early menopause that can be addressed.
Neuroplasticity may be reduced in early menopause, potentially impacting learning and adaptation abilities. This means you might find it harder to learn new skills or adapt to new situations. Understanding this connection can help you be more patient with yourself and seek appropriate support.
| Cognitive Function | Impact of Early Menopause |
|---|---|
| Memory | Potential decline in short-term memory |
| Concentration | Increased difficulty focusing |
| Learning | Possible challenges in acquiring new skills |
| Multitasking | Reduced efficiency in managing multiple tasks |
To support cognitive function and energy levels throughout the day, consider exploring a balanced breakfast meal plan. Proper nutrition can play a significant role in managing the cognitive symptoms of early menopause.
Skeletal Surprises
One of the less visible but critically important effects of early estrogen decline is accelerated bone density loss. This can have significant implications for your long-term health, increasing the risk of osteoporosis and fractures at a younger age than expected.
Estrogen plays a key role in maintaining bone mineral density by regulating osteoclast and osteoblast activity. When estrogen levels drop, the balance between bone formation and breakdown is disrupted, leading to net bone loss.
The rate of bone loss in early menopause can be up to 2-3% per year, compared to 0.5-1% in natural menopause. This accelerated loss means that women experiencing early menopause may be at risk for osteoporosis much earlier than their peers.
Early intervention with bone-strengthening strategies is crucial to mitigate long-term osteoporosis risk. This might include dietary changes, weight-bearing exercises, and in some cases, medication. Don’t wait until you’ve already lost significant bone density to take action.

Source: Unified Premier Women’s Care
From another perspective, some women report feeling empowered by the early onset of menopause. They view it as an opportunity to take charge of their health earlier in life, implementing lifestyle changes that benefit them in the long run. This proactive approach can lead to better overall health outcomes and a sense of control over the aging process.
The Progesterone Puzzle
While estrogen often takes center stage, progesterone’s role in early menopause shouldn’t be overlooked. This hormone significantly impacts your mood and sleep patterns, and its decline can lead to noticeable changes in these areas.
Progesterone acts as a natural anxiolytic and sedative, influencing GABA receptors in the brain. As progesterone levels drop, you might find yourself feeling more anxious or having trouble relaxing. This isn’t just stress – it’s a hormonal shift that can be addressed.
The ratio of estrogen to progesterone becomes imbalanced in early menopause, potentially exacerbating symptoms. This imbalance can lead to a range of symptoms that might seem unrelated but are actually interconnected.
Progesterone’s decline can affect the menstrual cycle before noticeable estrogen-related symptoms appear. You might notice changes in your cycle length or flow before experiencing classic menopausal symptoms like hot flashes.
Lisa, a 44-year-old teacher, found herself experiencing unexplained anxiety and insomnia. After consulting her doctor, she learned that these symptoms were related to declining progesterone levels, an early sign of menopause. Understanding this connection helped her seek appropriate treatment and lifestyle adjustments.
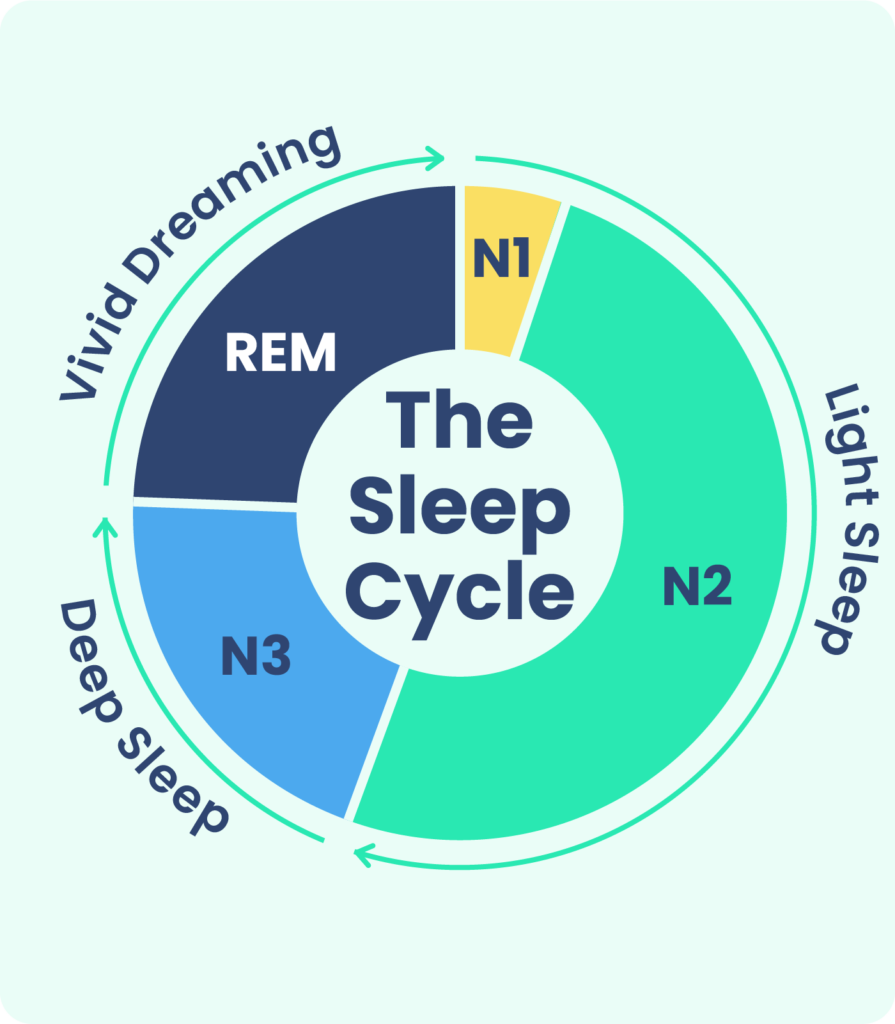
Sleep Cycle Shifts
You might find yourself tossing and turning more often, or waking up in the middle of the night. These sleep disturbances aren’t just annoying; they’re often directly linked to the hormonal changes of early menopause, particularly fluctuations in progesterone levels.
Progesterone influences sleep architecture, particularly REM and slow-wave sleep stages. As progesterone levels decline, you might notice that your sleep feels less restful or that you’re waking up more frequently during the night.
Decreased progesterone can lead to increased sleep latency and more frequent night awakenings. You might find it takes longer to fall asleep or that you’re more easily awakened by noises or disturbances.
The interaction between progesterone and melatonin production becomes disrupted in early menopause. This can lead to changes in your natural sleep-wake cycle, making it harder to maintain a consistent sleep schedule.
Source: Sleep Foundation
Emotional Rollercoaster
Mood swings, increased anxiety, or unexplained feelings of depression might catch you off guard. These emotional changes aren’t just “in your head” – they’re real and valid experiences tied to the hormonal shifts of early menopause.
Progesterone metabolites act on GABA receptors, influencing mood regulation and anxiety levels. As progesterone levels fluctuate, you might find yourself feeling more emotionally volatile or experiencing heightened anxiety.
The ratio of allopregnanolone (a progesterone metabolite) to other neurosteroids becomes imbalanced in early menopause. This imbalance can contribute to mood swings and feelings of emotional instability.
Fluctuations in progesterone levels can affect serotonin function, potentially contributing to mood instability. You might notice that your mood seems to change more rapidly or that you’re more prone to feelings of sadness or irritability.
Recent reports have highlighted various warning signs of early menopause, including vaginal dryness and other symptoms that might not immediately be associated with menopause [Punch]. Being aware of these less obvious signs can help in early identification and management of early menopause.
To support hormone balance and mood stability during early menopause, consider exploring a paleo diet meal plan. Nutrition can play a significant role in managing the emotional symptoms of early menopause.
The Ripple Effect: Systemic Changes
Early menopause doesn’t just affect your reproductive system; it creates a ripple effect throughout your body. Understanding these systemic changes is crucial for maintaining your overall health and preventing potential long-term issues.
Early menopause can accelerate age-related changes in multiple organ systems. This means that you might experience health changes typically associated with older age much earlier than expected. It’s not just about reproductive health – early menopause can affect your cardiovascular system, bones, and even your brain.
The interplay between hormonal changes and systemic health requires a holistic approach to management. It’s not enough to just treat individual symptoms; we need to look at how these changes are interconnecting and affecting your overall health.
[This video provides an overview of early menopause symptoms and their systemic effects, complementing the information in this section.]
Video Source: https://www.youtube.com/embed/_nMdn6EI6WA
Metabolic Metamorphosis
You might notice changes in your metabolism and body composition that seem to happen almost overnight. These shifts are a direct result of the hormonal changes associated with early menopause and can have significant impacts on your overall health.
Estrogen plays a role in glucose metabolism and insulin sensitivity. As estrogen levels decline, you might find that your body processes sugars differently, potentially increasing your risk of insulin resistance or type 2 diabetes.
The loss of estrogen’s protective effects on metabolism occurs earlier in women with early menopause. This means that metabolic changes typically associated with aging might occur sooner than expected.
Changes in body fat distribution, particularly increased visceral fat, can occur more rapidly in early menopause. You might notice that you’re gaining weight around your midsection, even if your diet and exercise habits haven’t changed.

Source: Liebert Pub
Insulin Resistance Risk
Your body’s ability to process insulin effectively may change, increasing your risk of developing insulin resistance. This shift can have long-term implications for your metabolic health and diabetes risk.
Estrogen influences pancreatic beta-cell function and insulin secretion. As estrogen levels decline, you might find that your blood sugar levels are less stable or that you’re more prone to energy crashes after meals.
The loss of estrogen’s protective effect on insulin sensitivity occurs earlier in early menopause. This means that you might need to be more vigilant about your blood sugar levels and insulin function at a younger age than you expected.
Increased visceral fat accumulation in early menopause can exacerbate insulin resistance risk. This type of fat, which accumulates around your organs, is particularly problematic for metabolic health.
To help manage insulin resistance and support metabolic health during early menopause, consider exploring a low carb meal plan. Proper nutrition can play a significant role in managing the metabolic changes associated with early menopause.
Muscle Mass Matters
You might notice a decrease in muscle strength or find it harder to maintain muscle mass. This accelerated loss of muscle tissue is a common but often overlooked aspect of early menopause.
Estrogen plays a role in muscle protein synthesis and satellite cell activation. As estrogen levels decline, you might find it harder to build or maintain muscle mass, even if you’re exercising regularly.
The anabolic effects of other hormones, such as growth hormone and IGF-1, may be reduced in early menopause. This can further contribute to the loss of muscle mass and strength.
Decreased muscle mass can impact metabolic rate and increase the risk of sarcopenia at a younger age. This loss of muscle tissue can have far-reaching effects on your overall health and functionality.
| Body Composition Changes | Impact of Early Menopause |
|---|---|
| Muscle Mass | Accelerated loss of lean muscle tissue |
| Fat Distribution | Increased visceral fat accumulation |
| Bone Density | Rapid decrease in bone mineral density |
| Metabolic Rate | Potential decrease in basal metabolic rate |
Cardiovascular Considerations
Early menopause can have significant impacts on your heart health and circulatory system. Understanding these changes is crucial for maintaining cardiovascular health and preventing potential issues down the line.
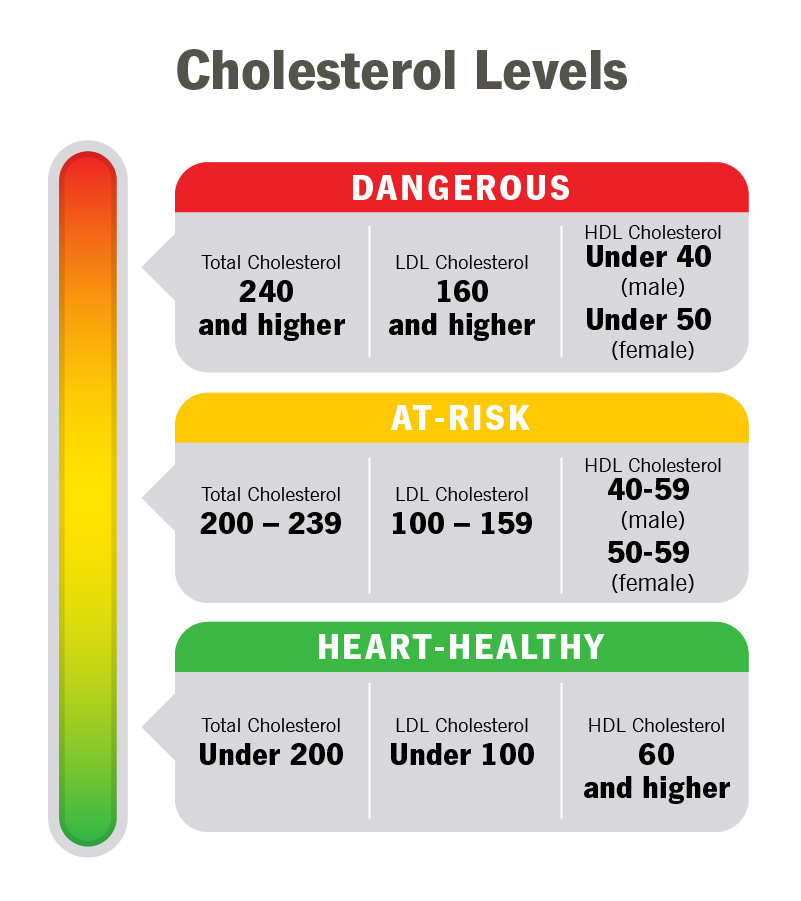
Estrogen has cardioprotective effects, including maintaining arterial flexibility and regulating cholesterol levels. As estrogen levels decline, you might find that your cardiovascular risk factors start to increase.
The loss of these protective effects in early menopause can accelerate cardiovascular risk factors. This means that you might need to start paying closer attention to your heart health at a younger age than you expected.
Early menopause may necessitate earlier I apologize for the confusion. I’ll continue from where I left off:
Early menopause may necessitate earlier and more aggressive cardiovascular risk management. This could involve lifestyle changes, dietary adjustments, and in some cases, medical interventions to protect your heart health.
Studies have shown that women with premature menopause have a 50% higher risk of coronary heart disease compared to women who experience menopause at the average age [Yale Medicine]. This statistic underscores the importance of proactive cardiovascular care for women experiencing early menopause.
Cholesterol Challenges
You might see changes in your cholesterol levels that seem out of sync with your diet and lifestyle. These shifts are often directly related to the hormonal changes of early menopause and can increase your risk of cardiovascular disease.
Estrogen helps maintain a favorable lipid profile by increasing HDL and decreasing LDL cholesterol. As estrogen levels drop, you might notice your cholesterol numbers moving in less favorable directions, even if your diet hasn’t changed.
The loss of estrogen’s effects on lipid metabolism occurs earlier in women with early menopause. This means you might need to start monitoring your cholesterol levels more closely at a younger age than you anticipated.
Changes in cholesterol ratios can occur more rapidly, potentially accelerating atherosclerosis risk. It’s not just about total cholesterol – the balance between different types of cholesterol becomes increasingly important.
Source: Cleveland Clinic
Blood Pressure Fluctuations
Your blood pressure readings might become more variable or trend upward. These changes are often linked to the hormonal shifts of early menopause and require careful monitoring and management.
Estrogen influences vascular tone and endothelial function, helping to regulate blood pressure. As estrogen levels decline, you might find that your blood pressure becomes less stable or starts to creep up.
The loss of estrogen’s vasodilatory effects can lead to increased vascular resistance in early menopause. This can make your blood vessels less flexible, potentially contributing to higher blood pressure.
Renin-angiotensin system activity may be altered in early menopause, affecting blood pressure regulation. This complex hormonal system plays a crucial role in blood pressure control, and its disruption can have significant effects.
To support cardiovascular health during early menopause, consider exploring a personalized meal plan. Proper nutrition can play a significant role in managing the cardiovascular changes associated with early menopause.
Navigating the New Normal
Adapting to early menopause requires a multifaceted approach. By implementing targeted lifestyle changes and exploring various management strategies, you can effectively address symptoms and promote overall well-being.
A personalized approach to early menopause management is crucial due to the variability of symptoms and individual health profiles. What works for one woman may not work for another, so it’s important to tailor your strategies to your specific needs and experiences.
Integrative strategies combining lifestyle modifications and medical interventions often yield the best outcomes. This might involve a combination of dietary changes, exercise routines, stress management techniques, and medical treatments.
Jennifer, a 46-year-old architect, initially struggled with the symptoms of early menopause. By working closely with her healthcare team, she developed a comprehensive management plan that included hormone therapy, regular exercise, and dietary changes. This personalized approach helped her regain control of her symptoms and maintain her quality of life.
Holistic Approaches to Symptom Management
Managing early menopause symptoms often requires a holistic approach. By addressing multiple aspects of your lifestyle, you can create a comprehensive strategy for symptom relief and overall health improvement.
Holistic approaches can address the interconnected nature of menopausal symptoms. For example, improving your sleep habits might also help with mood swings and energy levels.
Non-pharmacological interventions can complement medical treatments and may reduce the need for medication in some cases. These might include mindfulness practices, acupuncture, or herbal supplements.
Personalized holistic strategies can improve quality of life and potentially mitigate long-term health risks associated with early menopause. By taking a whole-person approach, you’re not just treating symptoms – you’re supporting your overall health and well-being.
Source: Baptist Memorial Health Care
Nutrition for Balance
Your dietary choices can play a significant role in managing early menopause symptoms. Focusing on nutrient-dense foods and specific dietary strategies can help alleviate symptoms and support overall hormonal balance.
Phytoestrogens in certain foods may help modulate estrogen receptor activity. While not a replacement for hormonal therapy, incorporating foods rich in phytoestrogens might help mitigate some menopausal symptoms.
Specific nutrients like calcium, vitamin D, and omega-3 fatty acids become increasingly important in early menopause. These nutrients support bone health, mood stability, and cardiovascular function – all crucial areas affected by early menopause.
Balancing macronutrients can help stabilize blood sugar and potentially reduce the frequency of hot flashes. Paying attention to the balance of proteins, carbohydrates, and healthy fats in your diet can have far-reaching effects on your menopausal symptoms.
Exploring a well-planned meal strategy can support your nutritional needs during early menopause. Proper nutrition is a cornerstone of managing menopausal symptoms and supporting long-term health.
Mind-Body Connections
The mind-body connection is particularly relevant in early menopause. Exploring stress-reduction techniques and mindfulness practices can help you manage both physical symptoms and emotional challenges.
Stress reduction techniques can help modulate cortisol levels, which interact with sex hormones. By managing stress, you’re not just improving your mental health – you’re potentially influencing your hormonal balance as well.
Mindfulness practices may improve vasomotor symptoms by affecting the autonomic nervous system. Techniques like meditation or deep breathing exercises might help reduce the frequency or intensity of hot flashes.
Regular mind-body practices can potentially improve sleep quality and reduce anxiety associated with early menopause. These practices offer a non-pharmacological approach to managing some of the most challenging aspects of early menopause.
Medical Interventions and Considerations
While lifestyle changes are crucial, medical interventions often play a key role in managing early menopause. Understanding the range of available treatments, their benefits, and potential risks is essential for making informed decisions about your care.
The risk-benefit profile of medical interventions may differ for women with early menopause compared to those with natural menopause. This means that treatments that might not be recommended for women experiencing menopause at the typical age might be appropriate for those with early menopause.
Individualized treatment plans should consider factors such as age, symptom severity, and personal health history. There’s no one-size-fits-all approach to managing early menopause – your treatment plan should be as unique as you are.
Regular monitoring and adjustment of medical interventions is often necessary due to the dynamic nature of early menopause. Your needs may change over time, so it’s important to maintain open communication with your healthcare provider.
Hormone Therapy: Weighing the Options
Hormone replacement therapy (HRT) is often a key consideration for women experiencing early menopause. Understanding the pros and cons of HRT can help you make an informed decision about whether it’s right for you.
The risk-benefit profile of HRT may be more favorable for women with early menopause compared to those with natural menopause. This is because the benefits of replacing lost hormones often outweigh the potential risks for younger women.
Different HRT formulations and delivery methods can be tailored to individual needs and risk factors. From pills to patches to creams, there are numerous ways to receive hormone therapy, each with its own set of benefits and considerations.
The duration of HRT use may need to be longer in early menopause to provide adequate protection against long-term health risks. While women experiencing natural menopause might use HRT for a shorter period, those with early menopause often need longer-term treatment to protect their bone and heart health.

Source: Herstasis
Alternative Therapies: Exploring Options
Non-hormonal treatments and complementary therapies can offer additional options for symptom relief. Exploring these alternatives can help you create a comprehensive management plan that aligns with your preferences and needs.
Certain herbal supplements may modulate estrogen receptors or affect neurotransmitters involved in menopausal symptoms. While research is ongoing, some women find relief from symptoms like hot flashes or mood swings with herbal remedies.
Acupuncture and other traditional medicine approaches may influence the hypothalamic-pituitary-ovarian axis. These therapies offer a different approach to managing menopausal symptoms, potentially providing relief without the use of hormones.
Mind-body interventions like cognitive-behavioral therapy can address the psychological aspects of early menopause. These approaches can be particularly helpful for managing mood changes, anxiety, or depression associated with early menopause.
Learning how personalized nutrition calculations can support your health goals during early menopause can be a valuable tool in your management strategy. Proper nutrition is a key component of managing early menopause symptoms and supporting overall health.
The Psychological Journey
Early menopause isn’t just a physical transition; it’s an emotional and psychological journey as well. Understanding and addressing the mental health aspects of this change is crucial for overall well-being.
The psychological impact of early menopause can be more pronounced due to its unexpected timing. You might find yourself grappling with emotions and life changes you weren’t prepared to face at this stage of your life.
Cognitive changes associated with early menopause can interact with emotional experiences, creating unique challenges. You might find that mood swings or anxiety are compounded by difficulties with memory or concentration, creating a complex web of psychological experiences.
Identity and Transition
Experiencing menopause earlier than expected can significantly impact your sense of self and identity. Navigating this transition involves not just managing physical symptoms, but also redefining your self-concept and life expectations.
Early menopause can trigger identity-related concerns typically associated with midlife, but at an earlier stage. You might find yourself questioning your role as a woman, your fertility status, or your place in society earlier than you anticipated.
The intersection of hormonal changes and psychological adaptation can create complex emotional experiences. You might feel like you’re on an emotional rollercoaster, with your sense of self shifting along with your hormones.
Developing new coping mechanisms and reframing life goals may be necessary to adapt to early menopause. This might involve reassessing your career plans, relationships, or personal aspirations in light of this unexpected life change.
Fertility Farewells
The premature loss of fertility can be one of the most emotionally challenging aspects of early menopause. Addressing these feelings and finding ways to cope with this unexpected change is an important part of the journey.
The grief process associated with fertility loss in early menopause may be more complex due to its unexpected nature. You might find yourself mourning not just the loss of fertility, but also the loss of time you thought you had to make family planning decisions.
Hormonal changes can interact with emotional processing, potentially intensifying feelings of loss. You might find that your emotions feel more intense or unpredictable as you navigate this grief.
Exploring fertility preservation options or alternative family-building strategies may be part of the coping process. While not right for everyone, understanding your options can help you feel more in control of your reproductive future.
Embracing a New Chapter
While early menopause brings challenges, it also offers opportunities for growth and self-discovery. Finding ways to reframe this experience positively can help you navigate this transition with resilience and optimism.
Positive reframing can influence neuroendocrine function, potentially impacting symptom experience. By changing how you think about early menopause, you might actually influence how you physically experience it.
Developing new interests or pursuits can stimulate neuroplasticity, which may help counteract cognitive changes. This is a great time to learn a new skill, take up a hobby, or pursue a passion you’ve always been interested in.
Building resilience through this experience can have long-term benefits for mental health and well-being. The coping skills and emotional strength you develop during this time can serve you well throughout the rest of your life.
Social and Relational Dynamics
Early menopause can affect your relationships and social interactions in various ways. Understanding these changes and developing strategies to navigate them is crucial for maintaining strong connections with others.
Hormonal changes can influence social cognition and interpersonal behavior. You might find that you’re more sensitive to social cues or that your social needs have changed.
The unique timing of early menopause may create a sense of being “out of sync” with peers, affecting social dynamics. You might feel like you’re going through experiences that your friends can’t relate to yet.
Changes in libido and sexual function can impact intimate relationships, requiring open communication and adaptation. This can be a challenging aspect of early menopause, but it’s important to address it openly with your partner.
Partner Communication
Open and honest communication with your partner is essential when navigating early menopause. Discussing your experiences, needs, and concerns can help strengthen your relationship and ensure mutual understanding and support.
Hormonal changes can affect mood and communication styles, necessitating new strategies for effective dialogue. You might need to be more explicit about your needs or feelings than you were before.
Educating partners about the physiological aspects of early menopause can improve empathy and support. The more your partner understands about what you’re going through, the better they can support you.
Addressing changes in sexual function and intimacy may require professional guidance and open discussion. Don’t hesitate to seek help from a therapist or counselor specializing in menopausal issues if you’re struggling in this area.
Peer Support and Understanding
Connecting with others who are experiencing early menopause can provide invaluable support and understanding. Building a network of peers facing similar challenges can help you feel less isolated and more empowered in your journey.
Peer support can positively influence stress hormone levels and immune function. Sharing your experiences with others who truly understand can have tangible benefits for your physical and emotional health.
Shared experiences can provide practical coping strategies and normalize the early menopause experience. You might learn tips and tricks for managing symptoms that you wouldn’t have thought of on your own.
Online communities can offer accessible support, particularly for those who may not have local resources. These virtual spaces can be a lifeline, providing 24/7 access to support and information.
Discovering how personalized meal plans can support your nutritional needs and overall well-being during early menopause can be a valuable part of your management strategy. Proper nutrition is a key component of managing early menopause symptoms and supporting overall health.
Premature Menopause: A Distinct Challenge
Premature menopause, occurring before age 40, presents an even more complex set of challenges. Understanding the unique aspects of this condition is crucial for those affected and requires specialized care and consideration.
Premature menopause affects approximately 1% of women under 40. While this might seem like a small percentage, it represents a significant number of women who are facing this unexpected life change at a very young age.
The health implications of premature menopause can be more severe due to the extended period of hormone deficiency. This means that women experiencing premature menopause might face even greater risks to their bone health, heart health, and overall well-being.
Genetic Factors and Autoimmune Connections
Premature menopause often has underlying genetic or autoimmune causes. Understanding these factors can help you make sense of your experience and guide appropriate treatment strategies.
Certain genetic mutations, such as those affecting the FMR1 gene, are associated with premature ovarian insufficiency. If you’re experiencing premature menopause, genetic testing might provide insights into the underlying cause.
Autoimmune disorders like thyroiditis or lupus can trigger premature menopause in some women. This connection between autoimmune conditions and premature menopause highlights the importance of comprehensive health screening.
Genetic testing and autoimmune screening may be recommended for women experiencing premature menopause. These tests can provide valuable information to guide your treatment plan and help you understand your overall health risks.
Familial Patterns
Your family history might hold clues about your risk for premature menopause. Recognizing patterns across generations can help you and your healthcare provider take proactive steps.
Premature menopause can have a hereditary component I apologize for the confusion. I’ll continue from where I left off:
Premature menopause can have a hereditary component, with a 6-fold increased risk in first-degree relatives. If your mother or sister experienced premature menopause, you might be at higher risk yourself. This information can help you and your healthcare provider be more vigilant about early signs and symptoms.
Epigenetic factors may influence the expression of genes related to ovarian function and menopause timing. This means that environmental factors and lifestyle choices might interact with your genetic predisposition to premature menopause.
Family history analysis can inform genetic counseling and testing decisions. Understanding your family’s health history can provide valuable context for your own experiences and help guide your healthcare decisions.
Chromosomal Abnormalities
Some cases of premature menopause stem from chromosomal issues. These genetic variations can affect ovarian function and lead to early onset of menopause symptoms.
Turner syndrome (45,X) is a common chromosomal cause of premature ovarian insufficiency. Women with Turner syndrome often experience premature menopause as part of their condition.
Fragile X premutation carriers have an increased risk of premature ovarian insufficiency. This genetic condition can impact ovarian function and fertility, often leading to premature menopause.
Karyotype analysis and specific genetic tests can identify chromosomal abnormalities related to premature menopause. These tests can provide crucial information about the underlying causes of your condition and help guide treatment decisions.
Long-Term Health Implications
Premature menopause can have far-reaching effects on your health. Understanding these potential impacts is crucial for developing a comprehensive long-term health strategy.
Women with premature menopause face an increased risk of osteoporosis, cardiovascular disease, and cognitive decline. The extended period of estrogen deficiency can impact multiple body systems, necessitating a proactive approach to health management.
The duration of estrogen deficiency is a key factor in determining long-term health risks. The earlier menopause occurs, the longer the body is without the protective effects of estrogen, potentially increasing health risks.
Tailored preventive strategies are essential to mitigate the increased health risks associated with premature menopause. This might involve more aggressive bone health measures, cardiovascular risk reduction strategies, and cognitive health interventions.
Bone Health Vigilance
Protecting your bone health becomes a top priority when facing premature menopause. Early intervention and ongoing monitoring are key to preventing osteoporosis and fractures.
Women with premature menopause may lose up to 20% of their bone density in the first 5-7 years after onset. This rapid bone loss underscores the importance of early and aggressive bone health interventions.
Bone density screening should begin earlier and occur more frequently in women with premature menopause. Regular DEXA scans can help track your bone health and guide treatment decisions.
Combination therapies including hormonal and non-hormonal interventions may be necessary for optimal bone protection. This might involve hormone replacement therapy, bone-building medications, and lifestyle interventions like weight-bearing exercise and calcium-rich diets.
Cardiovascular Risk Reduction
Your heart health requires special attention in the context of premature menopause. Implementing heart-protective strategies early can help offset the increased cardiovascular risks associated with prolonged estrogen deficiency.
Premature menopause is associated with a 50% higher risk of coronary heart disease. This increased risk makes cardiovascular health a top priority for women experiencing premature menopause.
Endothelial function and lipid profiles may be more severely affected in premature menopause. These changes can contribute to an increased risk of heart disease and stroke.
Aggressive management of cardiovascular risk factors is often recommended, potentially including hormone therapy. This might involve lifestyle changes, medications to manage cholesterol and blood pressure, and in some cases, hormone replacement therapy.
A low carb meal plan can support heart health during premature menopause. Proper nutrition plays a crucial role in managing cardiovascular risk factors and supporting overall health.
Recognizing the Signs: Beyond the Obvious
Early menopause can manifest in subtle ways that are easy to overlook. Becoming aware of these less common signs can help you identify the onset of menopause earlier and seek appropriate care.
Non-specific symptoms of early menopause can be mistaken for other health conditions, leading to delayed diagnosis. It’s important to consider menopause as a possible explanation for a range of seemingly unrelated symptoms.
The constellation of symptoms can vary widely between individuals, necessitating a personalized approach to diagnosis. What one woman experiences as a sign of early menopause might be completely different from another’s experience.
Sensory Shifts
Changes in how you perceive the world around you might be unexpected signs of early menopause. Paying attention to shifts in your sensory experiences can provide valuable clues about hormonal changes.
Hormonal fluctuations can affect neurotransmitter function, potentially altering sensory perception. You might notice changes in how you experience taste, smell, or even touch.
Changes in sensory processing may be subtle and gradual, requiring careful self-observation. Keeping a symptom diary can help you track these changes over time and identify patterns.
Taste Bud Transformations
You might notice changes in your food preferences or how certain flavors taste. These shifts in your palate can be linked to the hormonal changes of early menopause.
Estrogen influences taste receptor function and renewal. As estrogen levels decline, you might find that foods taste different or that your preferences for certain flavors change.
Altered taste perception can affect nutritional intake and food choices. You might find yourself craving different foods or struggling to enjoy foods you once loved.
Changes in saliva composition due to hormonal shifts may impact taste sensitivity. This can affect not just how foods taste, but also your overall oral health.
Olfactory Oscillations
Your sense of smell might become more sensitive or change in unexpected ways. These olfactory shifts can be subtle indicators of hormonal fluctuations associated with early menopause.
Estrogen modulates olfactory bulb function and olfactory epithelium regeneration. As estrogen levels change, you might notice that certain smells seem stronger or that you’re more sensitive to odors in general.
Changes in smell perception can interact with other menopausal symptoms, such as nausea or food aversions. You might find that certain smells trigger other symptoms or that your tolerance for strong odors changes.
Olfactory changes may precede more recognizable symptoms of early menopause. Paying attention to changes in your sense of smell could provide early clues about hormonal shifts.
Dermatological Clues
Your skin and hair can offer early signs of menopause that you might not immediately associate with hormonal changes. Paying attention to these dermatological shifts can provide valuable insights into your hormonal status.
Skin is a major target organ for sex hormones, with estrogen receptors present in various skin structures. As hormone levels change, you might notice differences in your skin’s texture, hydration, or overall appearance.
Changes in skin and hair can reflect systemic hormonal shifts before other symptoms become apparent. These changes might be subtle at first but can provide important clues about your hormonal health.
Collagen Collapse
You might notice changes in your skin’s texture or elasticity that seem premature for your age. These shifts in skin quality can be early indicators of the hormonal changes associated with menopause.
Estrogen plays a crucial role in maintaining skin collagen content and hydration. As estrogen levels decline, you might notice that your skin feels drier or less firm than it used to.
Accelerated collagen loss in early menopause can lead to increased skin laxity and fine line formation. You might notice more wrinkles or that your skin doesn’t “bounce back” as quickly as it used to.
Changes in skin barrier function may result in increased sensitivity or dryness. You might find that your skin reacts differently to products you’ve used for years or that you need to adjust your skincare routine.
Hair Havoc
Changes in your hair texture, growth patterns, or unexpected hair loss might catch you off guard. These hair-related changes can be subtle signs of the hormonal shifts occurring in early menopause.
The ratio of estrogen to androgens affects hair follicle function and the hair growth cycle. You might notice changes in the thickness or texture of your hair, or find that you’re losing more hair than usual.
Changes in hair density or the appearance of facial hair may occur due to altered hormone balances. Some women notice thinning hair on their scalp while experiencing increased hair growth on their face or body.
Scalp sensitivity and changes in hair texture can reflect broader hormonal shifts in early menopause. You might find that your scalp feels more sensitive or that your hair becomes drier or more brittle.
A paleo diet meal plan can support skin and hair health during early menopause. Proper nutrition plays a crucial role in maintaining healthy skin and hair during hormonal transitions.
Empowerment Through Knowledge
Taking control of your menopausal journey starts with arming yourself with accurate information. By becoming your own advocate and building a strong support network, you can navigate early menopause with confidence and resilience.
Informed patients often experience better health outcomes and higher satisfaction with their care. The more you understand about early menopause, the better equipped you’ll be to make decisions about your health and well-being.
Self-advocacy skills can lead to more personalized and effective management strategies. By actively participating in your healthcare, you can ensure that your unique needs and concerns are addressed.
Self-Advocacy in Healthcare
Becoming an active participant in your healthcare is crucial when navigating early menopause. Learning to effectively communicate with your healthcare providers ensures you receive the comprehensive care you need.
Patient-provider communication significantly impacts treatment adherence and outcomes. Being able to clearly articulate your symptoms, concerns, and preferences can lead to more effective treatment plans.
Shared decision-making models can lead to more satisfactory and effective treatment plans. By working collaboratively with your healthcare provider, you can develop a management strategy that aligns with your values and goals.
Health literacy specific to menopause can improve patient engagement and self-management skills. The more you understand about early menopause, the better equipped you’ll be to manage your symptoms and make informed decisions about your care.
Symptom Tracking Techniques
Keeping a detailed record of your symptoms can provide valuable insights for both you and your healthcare provider. Accurate symptom tracking helps in tailoring your treatment plan and monitoring progress over time.
Systematic symptom tracking can reveal patterns and triggers not immediately apparent. By consistently recording your symptoms, you might identify factors that exacerbate or alleviate your menopausal experiences.
Digital health tools can enhance the accuracy and convenience of symptom tracking. There are numerous apps and online platforms designed specifically for tracking menopausal symptoms.
Quantifiable data from symptom tracking can inform treatment decisions and medication adjustments. Having concrete information about your symptoms can help your healthcare provider make more informed decisions about your care.
Early Menopause Symptom Tracker:
- □ Hot flashes (frequency and intensity)
- □ Night sweats
- □ Mood changes
- □ Sleep disturbances
- □ Vaginal dryness
- □ Changes in libido
- □ Joint pain
- □ Cognitive changes (memory, concentration)
- □ Skin/hair changes
- □ Unusual sensory perceptions
Informed Decision-Making
Making choices about your health during early menopause requires careful consideration of various factors. Developing skills to research and evaluate treatment options empowers you to make decisions that align with your values and health goals.
Evidence-based decision aids can improve patient understanding of treatment options and outcomes. These tools can help you weigh the pros and cons of different treatment approaches.
Consideration of individual risk factors and preferences is crucial in personalizing treatment approaches. What works for one woman might not be the best choice for another, so it’s important to consider your unique circumstances.
Regular reassessment of treatment choices is important as symptoms and health status may evolve over time. Your needs may change as you progress through early menopause, so it’s important to periodically review and adjust your management strategy.
Personalized nutrition calculations can support informed decision-making during early menopause. Understanding how your nutritional needs change during this transition can help you make informed choices about your diet and lifestyle.
Building a Support Network
Creating a robust support system is invaluable when navigating early menopause. Connecting with others who understand your experience can provide emotional support, practical advice, and a sense of community.
Social support is associated with improved mental health outcomes and better coping strategies. Having people you can turn to for understanding and encouragement can make a significant difference in your menopausal journey.
Peer support can complement professional healthcare, providing unique insights and shared experiences. Other women who have gone through or are going through early menopause can offer practical tips and emotional support that complement your medical care.
Diverse support networks can address different aspects of the early menopause experience. This might include family, friends, support groups, and healthcare professionals, each offering different types of support.
Online Communities and Forums
Digital platforms offer accessible ways to connect with others experiencing early menopause. These online communities can provide round-the-clock support, information sharing, and a sense of belonging.
Online support groups can reduce feelings of isolation, particularly for those with rare or complex presentations. If you’re feeling alone in your experience, these communities can help you connect with others who truly understand.
Moderated forums can provide a balance of peer support and expert-vetted information. These spaces often have healthcare professionals or experienced moderators who can ensure the information shared is accurate and helpful.
Digital communities allow for anonymity, which may encourage more open discussion of sensitive topics. You might feel more comfortable discussing certain aspects of early menopause in an anonymous online setting.
Professional Counseling Options
Mental health support can be a crucial component of navigating early menopause. Exploring professional counseling options can help you develop coping strategies and address the emotional aspects of this life transition.
Cognitive-behavioral therapy has shown efficacy in managing mood symptoms associated with menopause. This type of therapy can help you identify and change thought patterns that might be contributing to emotional distress.
Mindfulness-based interventions can help in managing stress and improving overall well-being. These techniques can be particularly helpful for managing the physical and emotional symptoms of early menopause.
Specialized menopause counselors can provide targeted support for the unique challenges of early menopause. These professionals have specific training in menopausal issues and can offer tailored strategies for coping with this transition.
As we’ve explored the multifaceted aspects of early menopause, it’s clear that nutrition plays a crucial role in managing symptoms and maintaining overall health. This is where MealstoGlow can make a significant difference in your journey. Our tailored meal plans are designed to support hormonal balance, bone health, and cardiovascular wellness – all key concerns for women experiencing early menopause.
MealstoGlow’s meal plans incorporate foods rich in phytoestrogens, calcium, and omega-3 fatty acids. These nutrients can help support your body during the hormonal changes of early menopause.
Our recipes are crafted to help stabilize blood sugar levels, potentially reducing the frequency of hot flashes. By focusing on balanced meals with complex carbohydrates, lean proteins, and healthy fats, we aim to support stable energy levels throughout the day.
MealstoGlow offers customizable options to address individual nutritional needs associated with early menopause. We understand that every woman’s experience with early menopause is unique, and our meal plans can be tailored to your specific needs and preferences.
Ready to take control of your nutrition during this important life transition? Visit MealstoGlow.com to explore our menopause-friendly meal plans and start your journey towards balanced, supportive nutrition today.
Learnings Recap
- Early menopause at 45 affects multiple body systems and requires a comprehensive management approach
- Recognizing subtle signs and symptoms is crucial for early intervention and better health outcomes
- A combination of lifestyle changes, medical interventions, and psychological support can effectively manage early menopause
- Building a strong support network and becoming an informed self-advocate are key to navigating this life transition
- Nutrition plays a vital role in managing early menopause symptoms and maintaining long-term health
Early Menopause Action Plan:
- Health Assessment:
□ Schedule comprehensive health check-up
□ Undergo hormone level testing
□ Assess bone density and cardiovascular health - Symptom Management:
□ Implement symptom tracking system
□ Explore hormone therapy options with healthcare I apologize for the confusion. I’ll continue from where I left off:□ Explore hormone therapy options with healthcare provider
□ Investigate non-hormonal treatments for specific symptoms - Lifestyle Adjustments:
□ Develop a personalized nutrition plan
□ Establish a regular exercise routine
□ Implement stress reduction techniques
□ Optimize sleep hygiene - Support Network:
□ Join a menopause support group
□ Educate family and friends about early menopause
□ Consider professional counseling - Ongoing Education:
□ Stay informed about latest menopause research
□ Attend menopause-focused workshops or seminars
□ Regularly review and update management strategies
By following this action plan and utilizing the resources available, including the nutritional support offered by MealstoGlow, you can navigate early menopause with confidence and maintain optimal health throughout this transition and beyond.

Add comment